
Magnetic resonance imaging is a diagnostic method that provides a detailed picture of the nature of pathological changes in any area of the human body.
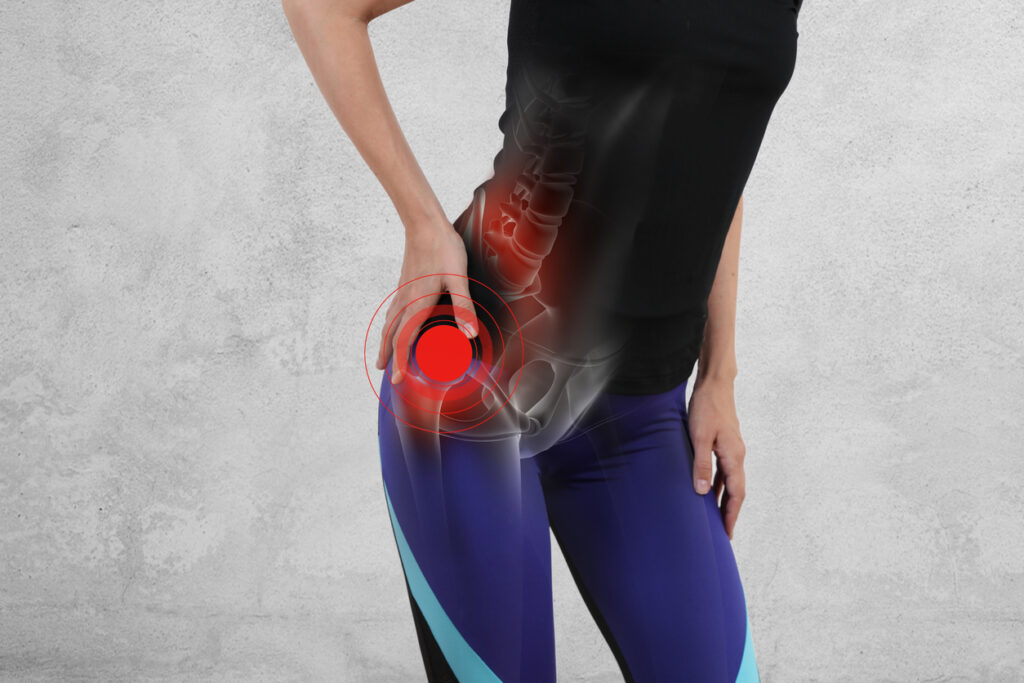
In orthopedic practice, MRI of the hip joint is most often performed to clarify the causes of coxalgia – pain syndrome in the joint. The method of research does not involve the use of ionizing radiation, which is especially relevant for children and pregnant women. The process of creating clear images, which can be magnified and viewed in volumetric view, is based on magnetic resonance and computer technologies. Contrast enhancement is used to improve imaging capabilities. The diagnostic value of photos obtained after gadolinium injection is comparable to the results of arthroscopy – an invasive study with penetration into the joint cavity with surgical instruments.
How is the MRI of the hip joint done? Scans are performed on machines with different magnetic field strengths. The doctor can choose the programs independently depending on the clinical objectives. This is relevant if it is not initially clear what is causing the pain syndrome: pelvic organ pathology or joint pathology. Multiparametric sequences are used in standard situations.
Diseases of the hip joint on MRI
Source: vanthielmd.com
Magnetic resonance scans are used to diagnose a number of pathological conditions. What does an MRI scan of the hip joint show? The scans visualize
- Femoroacetabular impingement syndrome.
A mechanical conflict between the femoral head/neck and the edge of the acetabulum is caused by single or bilateral bone defects of congenital or acquired origin. Modified components of the articulation cause dysfunction of the limb through collision during movement. Pathological friction of the bones contributes to the growth of osteophytes on the background of constant traumatization of the acetabular lip. If the disease is not diagnosed in time and treatment is not started, the latter will eventually rupture, and the cartilage tissue of the articulating bones will be destroyed. Such mechanical conflict often contributes to the formation of coxarthrosis and is accompanied by progressive pain syndrome.
MRI of the hip joint in femoroacetabular impingement syndrome shows the possible causes of the disease:
- congenital malformations;
- complications after trauma and surgical interventions;
- concomitant avascular necrosis of the femoral head;
- inflammatory processes in the synovial sac;
- osteochondropathy (Perters disease);
- epiphysiolysis (Salter-Harris fracture);
- Atrophied muscles around the articulation, etc.
In a severe form of diabetes mellitus with circulatory disorders, regular physical overload, concomitant diseases of the musculoskeletal system and connective tissue (arthritis, gout, systemic lupus erythematosus, etc.), destruction of bone and cartilage structures is found.
Osteoarthritis. A long-standing pathological process leads to the complete loss of function of the hip joint due to the destruction of all components of the joint. Changes in bone tissue, ligaments, blood vessels, cartilage, and surrounding muscles can be seen on MRI with contrast. Involvement of nerve bundles causes persistent pain in the hip. Predisposing factors include:
- endocrine disorders;
- Exercise of heavy sports;
- obesity;
- Associated arthritis, arthrosis, etc.
The disease has three degrees of severity. Hip MRI shows changes at an early stage, when it is possible to prevent/slow the progression of the pathology with the help of medication therapy.
- Avascular necrosis of the femoral head.
Development of avascular necrosis is caused by prolonged disruption of nutrition of the hip joint against the background of blood thickening, thrombosis, compression, twisting of the vessels. The ischemia creates voids in the bone tissue, leading to deformation and cartilage detachment. Clinical manifestations are nonspecific, causing difficulties in diagnosis. There are many provoking factors:
- trauma;
- prolonged hormone therapy;
- intoxication;
- Exposure to ionizing radiation, etc.
Early changes are not visible in X-rays or ultrasound. Hip MRI is one of the most effective ways to identify the disease in its early stages.
- Tumors.
Both benign and malignant tumors can develop in the hip joint. The MRI photo shows the presumptive nature of the tumor. Verification of the diagnosis requires a biopsy. Pain is seen when nerve endings, boundary tissues, and vessels are compressed, which is the case with any tumor, so the absence of symptoms should not delay MRI. Primary bone neoplasms are better diagnosed by CT scan, MRI is more suitable for demonstrating soft tissue changes.
Hip MRI: indications and contraindications

Source: medicalnewstoday.com
Endoprosthesis can cause defects in the images, so X-ray diagnostic methods are preferred.
MR tomography is performed in case of ambiguous results of computer scanning, radiography, ultrasound. The method is suitable for dynamic observation: for medical indications there are no restrictions on the number of MRI scans. Clinical manifestations in a number of pathological processes are similar, and extended diagnostics is required to determine the exact genesis of symptoms. Indications for hip MRI include:
- Prolonged pain syndrome, unexplained claudication, discomfort during walking and/or at rest, limitation of range of motion in the joint;
- absence of effect/short-term improvement against the background of therapy;
- assessment of post-traumatic complications – in an emergency situation, the search begins with CT scan;
- primary detection of disease – inflammation, destruction, tumor pathology, congenital anomalies, infectious lesion, degenerative-dystrophic processes, etc;
- examination before surgery and after surgical intervention – endoprosthetics, etc;
For pain associated with neuralgia, MRI of the hip joints shows normal, the study is performed to differentiate the processes.
Contraindications to MRI scanning:
- presence of implanted devices in the body – myo-, neuro-, pacemaker, defibrillator, insulin pump, permanent hearing prosthesis, vascular clips made of metal with paramagnetic properties, Ilizarov apparatus, etc;
- Pregnancy in the first trimester;
- Children under one month of age;
- obesity with body weight over 120 kg (for scanners with closed contour);
- severe well-being of the patient caused by an acute condition: pain syndrome against the background of trauma, heart attack, stroke, etc;
- Inability to stay in the supine position for a long time;
- some mental and neurological pathologies – alcohol delirium, epilepsy, claustrophobia, Parkinson’s disease, Alzheimer’s (MRI is done under hospital conditions under sedation).
Study with contrast is not available for patients with a history of allergic reactions to gadolinium, terminal renal failure, and pregnant women of any term. Permanent dental structures – veneers, posts, braces, titanium endoprostheses do not prevent MRI scanning
How do I get an MRI of a hip joint?

Source: hueftspezialist.de
To improve the signal-to-noise ratio, the problem area should be as close to the center of the table as possible
Magnetic resonance imaging of the mentioned joint is performed on different machines. Images obtained on the equipment with a closed contour are more informative. The best option is to have an MRI scan on a closed scanner with magnetic field strength from 1.5 Tesla. Low-power units are used for screening diagnostics of athletes, in the absence of complaints. More info on the site https://mricfl.com.
The patient arrives at the clinic 20 minutes before the examination. After paperwork is done and items containing metal are deposited, the X-ray technician places the patient on the CT scanner table.
During the diagnostic procedure, one or two hip joints may be looked at, which depends on the indications: systemic diseases imply a complex examination of several areas.
The patient is laid on his back, with the big toes brought together to allow rotation of the hip joints. A hamstring roll and soft fixation of the extremities with straps are used to prevent accidental movements. A coil is placed over the area of interest. When contrast is planned, a catheter is inserted into the ulnar vein and an automatic injector is connected: at a preset time the intensifying agent will be delivered into the body.
After evaluating the targeted images, the radiologist chooses the right MRI sequences. The diagnostic process is monitored by the medical staff through a window from a nearby room, and communication is carried out via a speakerphone. If the patient’s condition worsens, the scanning can be paused; the patient has a special button at hand. After the scan is completed, the patient is normally given a conclusion and a disk with a record of the diagnostic procedure. The video can be opened with a program that supports the dicom format.
How to prepare for a hip MRI?

Source: medicover.hu
No special measures are required, it is enough to put away metal objects (keys, coins, etc.), payment cards, remove jewelry, watches, wear loose clothing without zippers and rivets. Take a package of documents with you: passport, descriptions of the results of previous diagnostics, doctor’s referral, medical policy (if the payment will be made through an insurance company).
The injection of contrast into the body very rarely causes clinically significant side effects, but in 8-10% of cases vegetative reactions – salivation, dizziness, nausea, etc. – are recorded. To prevent such phenomena it is necessary to have a snack 15 minutes before leaving the house.
For women during the lactation period, preparation for MRI of the hip with contrast implies milk reserve for several feedings. An intensified drinking regimen after the diagnostic procedure will help to get rid of gadolinium chelates more quickly.
How is a hip MRI performed if internal organs also need to be looked at? If there is suspicion of possible pathology of the uterus, appendages, prostate, seminal vesicles, supporting pain syndrome, preparation for the study involves cleansing the bowel and eliminating flatulence. The bladder is evaluated when it is full.